by Ryan Christenson and Daniel Agyemang
Major depressive disorder introduction
According to the American Psychiatric Association, major depressive disorder (MDD) is a common and serious medical illness that negatively affects how you feel, think, and act.1 Symptoms of major depressive disorder include, but are not limited to, feelings of sadness, loss of interest in activities once enjoyed, sleep disorders, thoughts of suicide, feeling worthless or guilty, loss of energy or fatigue, and changes in appetite (weight loss or gain unrelated to dieting).2,3
In 2019, one in five adults (18.5%) aged 18 and older experienced symptoms of depression in the past two weeks in the United States (U.S).4
Clinical depression in Utah has been consistently higher than the national average since 2011.5 The age-adjusted prevalence of doctor-diagnosed depression among adults in Utah in 2019 was 23.0% compared to the national prevalence of 19.1%.6 Inequities were even more pronounced in 2019 across gender (29.3% in women and 16.5% in men) and household incomes (33.8% for <$25,000, 27.3% for $25,000 -$49,999, 21.1% for $50,000-$74,999, and 19.0% for income >$75,000).5,6
Analysis overview
This DataByte examines claim rates and allowed amounts for January 2019-April 2021 where major depressive disorder was the first-, second-, or third-listed diagnosis (ICD-10 code F33), using the Utah All Payers Claims Database (APCD), a database containing information about insurance plan members, their insurance plan coverage, and insurance claims from payers throughout Utah. APCD data for calendar year 2021 was partially complete at the time of this study, therefore the claims and coverage data in this study extend through April 2021.
Claim rates
Due to the fluctuations in the number of members covered by medical insurance over time, we opted to use claim rates instead of claim counts. The claim rate metric represents the rate of major depressive disorder-related claims within a time period per 1000 member months of medical insurance coverage over the same time period. The member month unit represents one member with coverage for a one-month period. All of the claims in the study were for professional or facility encounters; no prescription claims were included.
To better understand how major depressive disorder impacts various sub-populations, we reviewed claim rates with respect to four different groupings of variables:
- Monthly claim rates
- Claim rates grouped by gender and age group
- Claim rates grouped by gender and place of service
- Claim rates grouped by patient geographic classification (urban or rural) and place of service
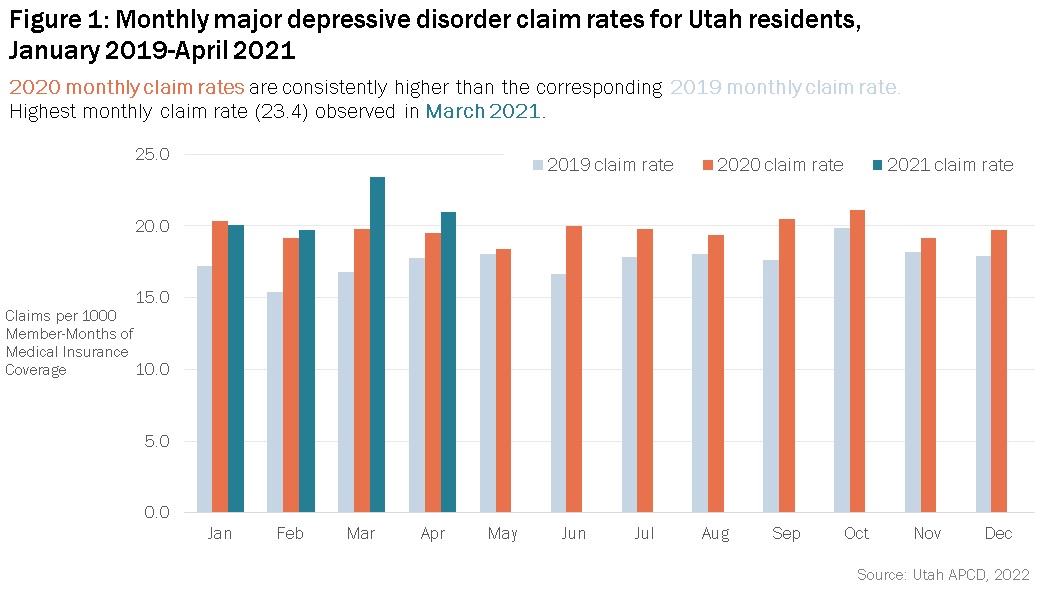
The claim rates throughout the year are steady, although 2019 and 2020 rates peaked in October. Overall the highest rate (23.4 claims per 1000 member months) occurred in March 2021. Monthly medical claim rates for the same month generally increased throughout the study period.
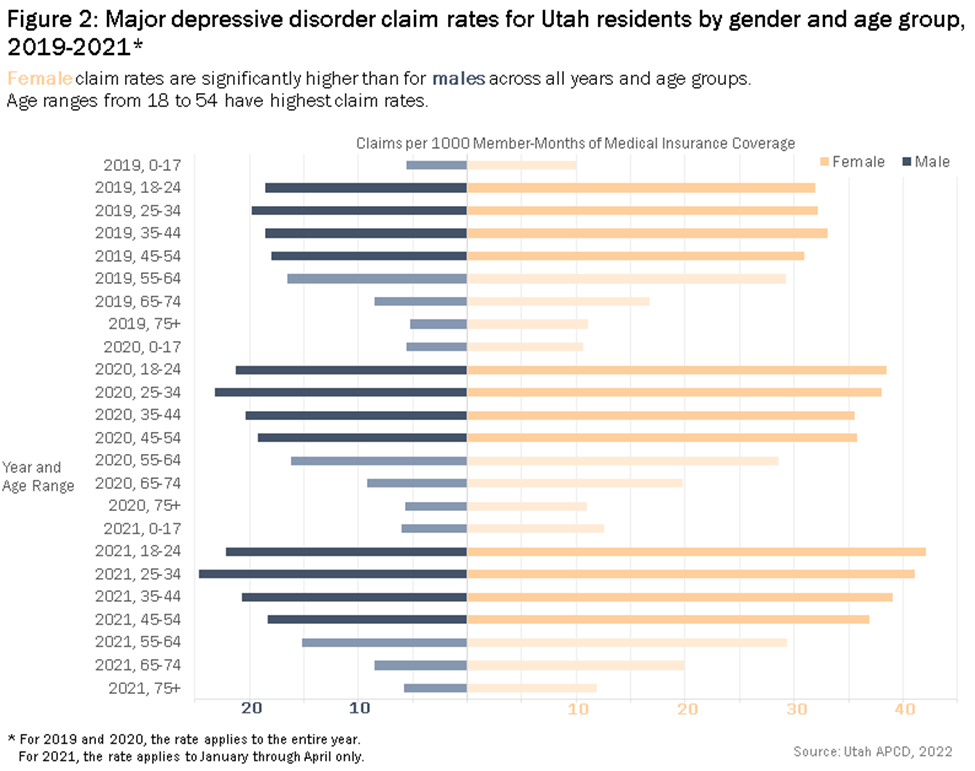
The general upward trend in claim rates from 2019 to 2021 noted in Figure 1 applies also to many individual gender and age groups. Female claim rates were significantly higher than for males across all years and age groups; the claim rates for males varied from 43% to 62% of the claim rate for females.
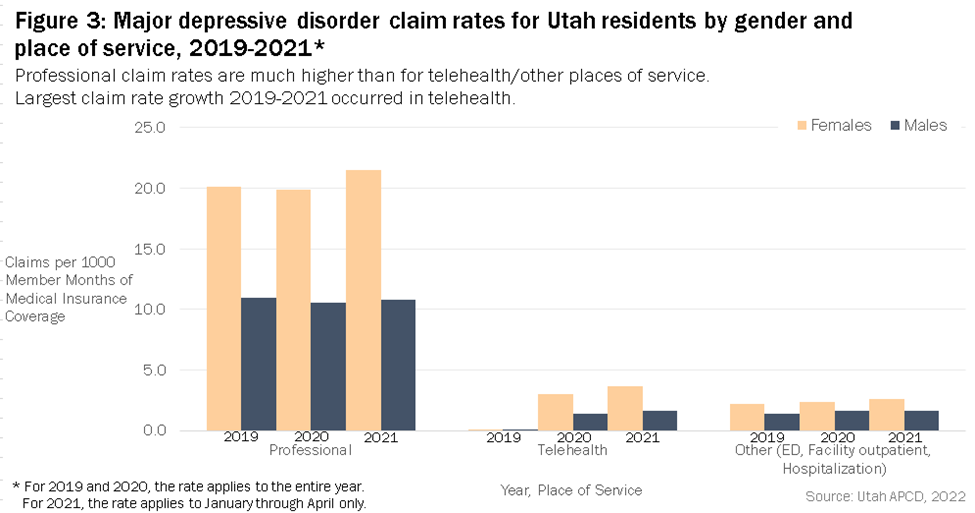
For services received in professional healthcare settings, major depressive disorder claim rates for females had a modest increase from 2019 to 2021, while male rates stayed almost the same. In 2020 and 2021, telehealth grew significantly as a means to provide healthcare to patients with major depressive disorder. Other healthcare settings (emergency department, facility outpatient and hospitalization) saw a modest increase in claim rates from 2019 to 2021.
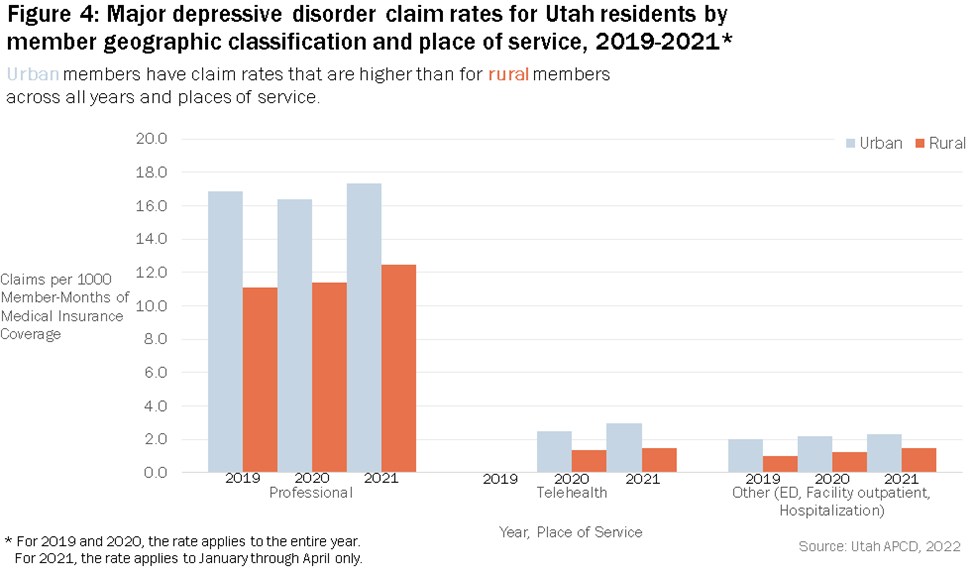
For services received in professional healthcare settings:
- Major depressive disorder claim rates for both urban and rural patients increased from 2019 to 2021.
- While rural patient claim rates are lower than urban rates in all three years, the rural rates as a percentage of urban rates increased from 66% to 72%.
Similar to patterns observed in Figure 3, significant claim rate increases in telehealth settings were observed for both urban and rural patients.
Average allowed amount
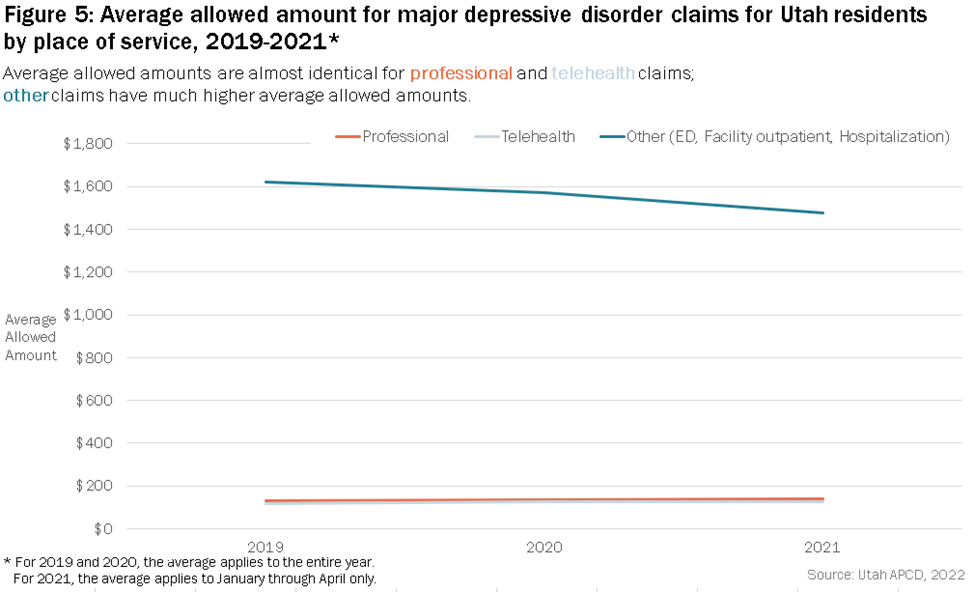
The allowed amount is the maximum amount a plan will pay for a covered health care service. The average allowed amounts for major depressive disorder-related claims for services in professional and telehealth settings are almost identical and change very little throughout 2019 to 2021. The average allowed amounts for services in other settings are much higher as they include emergency department visits and hospitalizations.
Conclusion and summary
Major depressive disorder affects many Utahns. Recent years have seen some difficult challenges (such as the global COVID-19 pandemic, social unrest, and natural disasters), which may relate in some degree with claim rates related to major depressive disorder and ways in which Utahns seek support and treatment. Claim rates related to major depressive disorder increased from 2019 to 2020; while this may be viewed as troubling in one sense, it also may be positive in the sense that more people are receiving help. Fortunately, many helpful resources are available, including telehealth services, standard in-person professional services, and the resources noted in the “Helpful resources for major depressive disorder” section below. Males in all age groups have claim rates substantially lower than their female counterparts; and rural Utahns have claim rates substantially lower than their urban counterparts.
Related issues this study did not examine include
- Unmet demand for mental health services, leading to longer wait times for such services
- Need for more mental health practitioners
While APCD data could be helpful in examining such issues, other data sources would also be helpful.
Helpful resources for major depressive disorder
Utah residents who are dealing with major depressive disorder have many resources available to them. Below are just a few resources including websites, smartphone apps, and telephone or text lines. The list is subdivided by severity, with self-help, prevention, or information type resources toward the top and crisis or intervention type resources toward the bottom.
Review your own health insurance plan’s coverage, resources, and providers with respect to mental health; also consider workplace leave policies.
https://211utah.org/index.php/mental-health
https://medlineplus.gov/depression.html
https://web-ui.mystrength.livongo.com/go/udhs/utahdhs
https://www.nami.org/About-Mental-Illness/Mental-Health-Conditions/Depression
https://www.nami.org/Support-Education/Support-Groups
Huntsman Mental Health Institute Support Line (Warm Line): 801-587-1055
National Help Line 800-662-HELP
https://www.samhsa.gov/find-help/disorders
Huntsman Mental Health Institute Crisis Line and Mobile Outreach Team: 801-587-3000
Utah Crisis Line 800-273-TALK
National Suicide Hotline 800-784-2433
References
1. Association AP. Diagnostic and Statistical Manual of Mental Disorders (DSM-5). Fifth ed2013.
2. Association AP. Depression. 2021; https://www.psychiatry.org/patients-families/depression/what-is-depression. Accessed 12/04/2021.
3. Lopez Molina MA, Jansen K, Drews C, Pinheiro R, Silva R, Souza L. Major depressive disorder symptoms in male and female young adults. Psychol Health Med. 2014;19(2):136-145.
4. Villarroel MA, Terlizzi EP. Symptoms of Depression Among Adults: United States, 2019. NCHS Data Brief. 2020(379):1-8.
5. AHR. Health Rankings Analysis of CDC, Behavioral Risk Factor Surveillance System. 2021; https://www.americashealthrankings.org/explore/annual/measure/Depression_a/state/UT. Accessed 12/04/2021.
6. IBIS-Utah. Health Indicator Report of Depression: Adult Prevalence. 2020; https://ibis.health.utah.gov/ibisph-view/indicator/view/Dep.html. Accessed 12/04/2021.